Pregnancy is a remarkable journey marked by profound physical and emotional transformations. One significant aspect is the cascade of hormonal fluctuations that accompany the gestational process. These hormonal shifts, while essential for nurturing and sustaining the developing fetus, can also deeply impact a woman’s mental state, potentially leading to postpartum depression (PPD).
During pregnancy, estrogen and progesterone levels surge, often reaching levels far beyond those experienced in a woman’s non-pregnant state. These hormones play crucial roles in regulating mood, appetite, and sleep patterns. However, the sudden fluctuations and eventual decline in these hormones after childbirth can disrupt the delicate balance, leaving some women vulnerable to PPD.
Other factors such as stress, lack of social support, previous history of depression, and childbirth complications can exacerbate the risk of developing PPD. The emotional and physical demands of caring for a newborn, coupled with sleep deprivation, can further exacerbate these challenges.
What is Postpartum Depression?
Postpartum depression (PPD) is a mood disorder that affects some women after childbirth. It’s characterized by persistent feelings of sadness, anxiety, and hopelessness that interfere with daily functioning. PPD typically manifests within the first few weeks after delivery but can occur anytime during the first year postpartum.
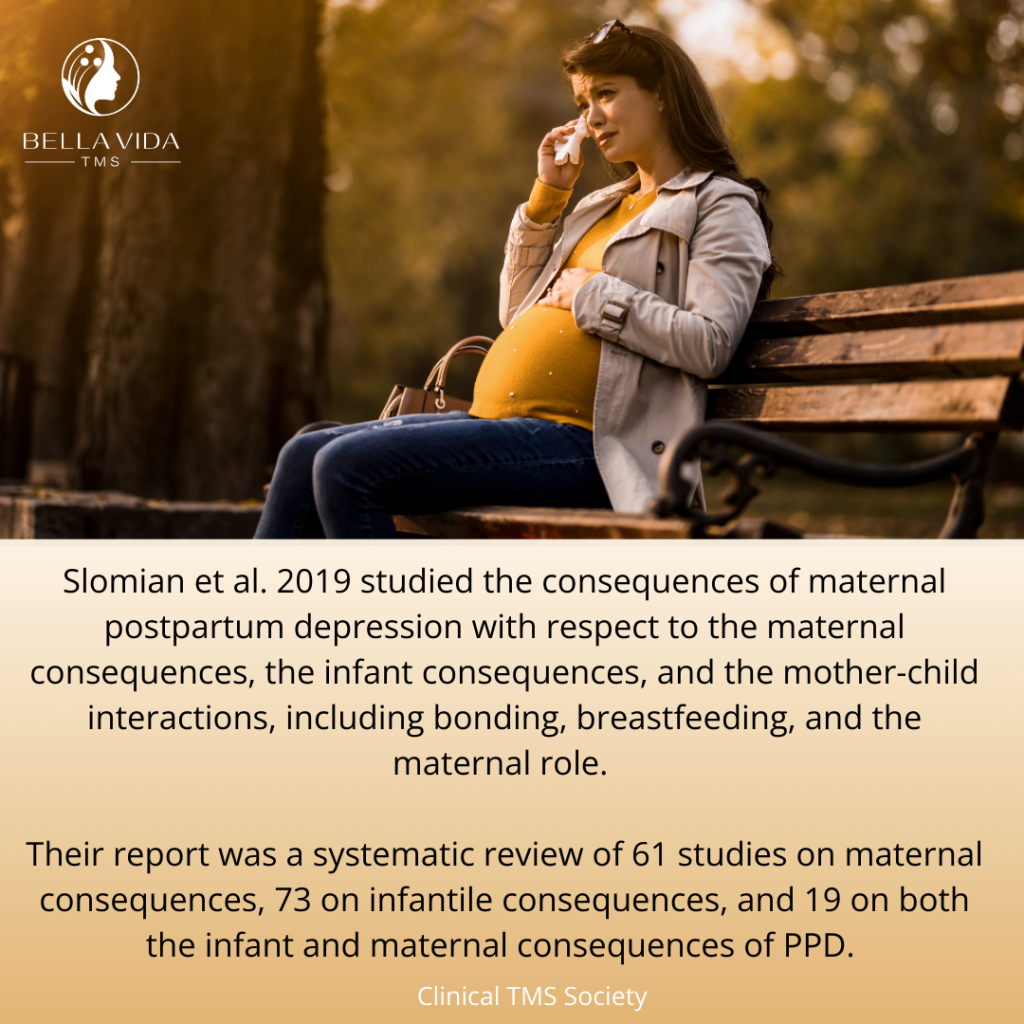
PPD not only impacts the mother’s emotional well-being but also affects her ability to care for and bond with her baby. Mothers with PPD may experience difficulty bonding with their infant, have trouble sleeping or eating, and feel overwhelmed by the responsibilities of motherhood. This can lead to strained relationships and feelings of guilt or inadequacy.
PPD can also have adverse effects on the baby’s development and well-being. Infants of mothers with untreated PPD may have trouble with emotional regulation, cognitive development, and forming secure attachments. Thus, it’s essential to recognize and address PPD promptly to ensure the well-being of both the mother and the baby.
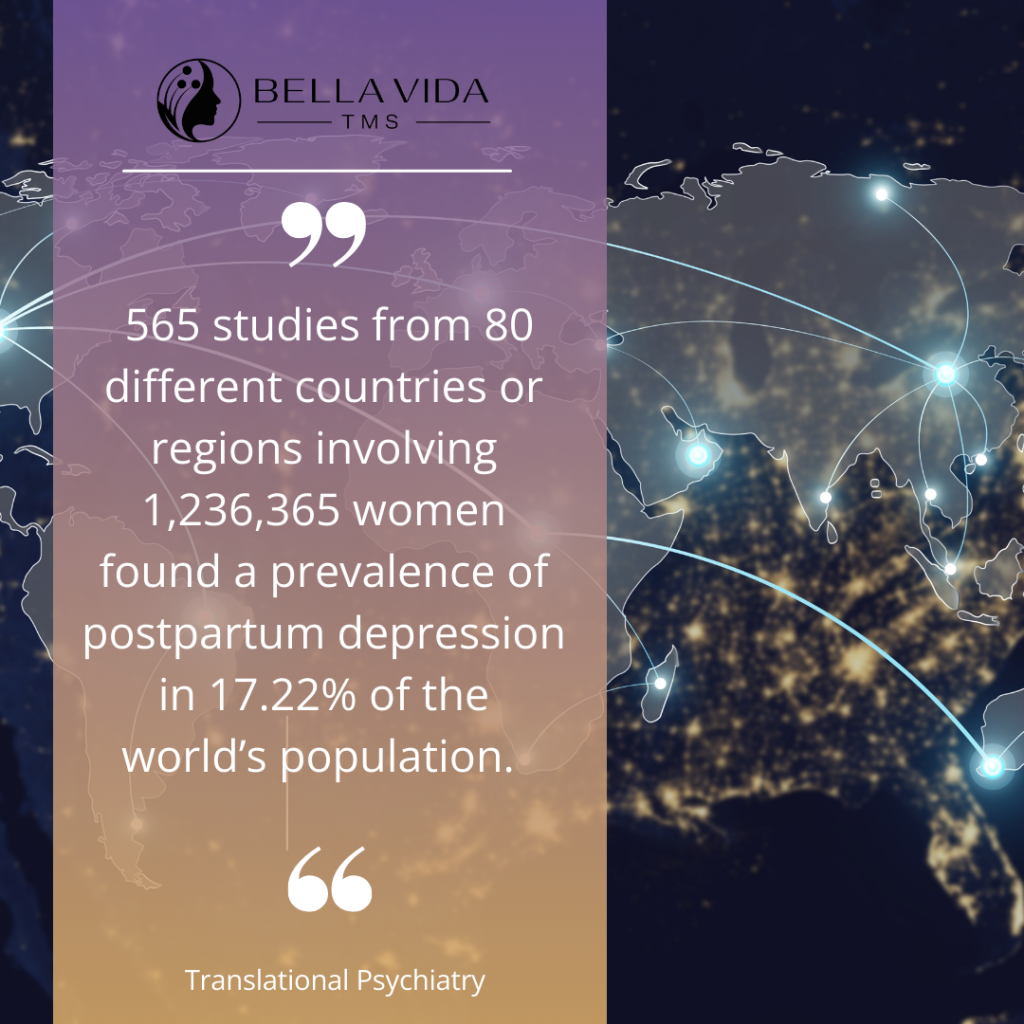
One scientific study suggests that major depression postpartum affects around 7% of all women, whereas the inclusion of minor depression raises this rate to 19%. However, these numbers may be underestimated; the prevalence of the disorder is up to 60% in certain developing countries, which seldom receive the same attention as developed countries based on international epidemiological studies.
Treating Major Depressive Disorder with Medication
Postpartum depression (PPD) is a treatable condition, and several effective interventions are available to support mothers in managing their symptoms and promoting recovery.
Therapy, particularly cognitive-behavioral therapy (CBT), is a common treatment for PPD. CBT helps mothers identify negative thought patterns and develop coping strategies to address them, leading to improved mood and functioning.
Medication can also be prescribed to alleviate symptoms of PPD. Selective serotonin reuptake inhibitors (SSRIs), such as sertraline and fluoxetine, are commonly used antidepressants considered safe for breastfeeding mothers. These medications work by increasing the levels of serotonin in the brain, which can help regulate mood and reduce symptoms of depression.
An article published in Clinical TMS Society in 2022 reported that while antidepressant therapy is frequently used to treat postpartum depression, they can take time to be effective and are not without concerns and side effects during pregnancy and while breastfeeding. Many patients are unwilling to take antidepressants due to fears of weight gain or sexual dysfunction.
In some cases, a combination of therapy and medication may be recommended for optimal symptom management. It’s essential for mothers to work closely with their healthcare providers to determine the most suitable treatment approach based on their individual needs and preferences.
Additionally, lifestyle modifications, such as regular exercise, adequate sleep, and social support, can complement formal treatment and promote overall well-being. By addressing PPD through a holistic approach, mothers can effectively manage their symptoms and nurture a positive postpartum experience for themselves and their babies.
PPD Medication and Breast Milk
Medications used to treat postpartum depression (PPD), such as selective serotonin reuptake inhibitors (SSRIs), can pass into breast milk in varying amounts. While many SSRIs are considered safe for breastfeeding, there’s still a risk of exposing the baby to the medication. This exposure may lead to side effects in infants, including irritability, agitation, poor feeding, and sleep disturbances. Healthcare providers carefully weigh the benefits of treatment for the mother against the potential risks to the baby when prescribing medications for PPD during breastfeeding, often opting for the safest options with minimal impact on the infant.
TMS and Postpartum Depression: Proof is in the Research
Transcranial Magnetic Stimulation (TMS) therapy offers a non-invasive, medication-free alternative for treating postpartum depression (PPD) without harming the child. By using magnetic pulses to stimulate nerve cells in the brain’s mood-regulating regions, TMS effectively alleviates depressive symptoms in mothers. Unlike medication, TMS doesn’t pass into breast milk, eliminating the risk of exposure to the infant. TMS provides a safe and effective option for managing PPD, empowering mothers to prioritize their mental health while nurturing their newborns.
A research study published in Neuropsychiatric Disease and Treatment in 2012 found that the active rTMS group showed a positive response to treatment, with a reduction of at least 30% in HDRS/17 and EPDS scores at week 6 (after 2 weeks of follow-up). They also observed marginal cumulative effects of rTMS on affective, social, and cognitive dimensions from week 4 to week 6.
Clinical TMS Society found one of the first reported rTMS treatments for postpartum depression in 1999. One of the first reports of rTMS in postpartum depression reported was Ogden et al.

In 1999, a 40-year-old female with a previous episode of postpartum depression developed depression again after her 2nd child. She received 20 Hz TMS at 100% MT of 1200 pulses to the left prefrontal cortex for 13 treatments along with citalopram and risperidone. She had documented improvement on her Hamilton Depression Rating Scale-17, the Beck Depression Inventory, and a Visual Analogue Scale. The study revealed her HDRS-17 improved from 29 to 3. Her Beck Depression Inventory improved from 48 to 13. And, the Visual Analogue Scale from 8.2 to 3.4.
Most recently, Cox et al. 2020 treated six patients with postpartum depression using 20 sessions left dorsolateral prefrontal cortex of 10 Hz frequency, 120% MT, for four seconds of stimulation and 26 seconds rest for 3000 pulses. The Beck Depression Inventory, the Edinburgh Postnatal Depression Scale and State-Trait Anxiety Inventory scores, all of which declined over the four weeks of treatment. Four of the six achieved remission, and two responded based on the EPDS. Using BDI scores, only one achieved remission. There was no disruption in lactation with TMS treatment.
PrTMS therapy, or Personalized repetitive Transcranial Magnetic Stimulation, is tailored specifically for mothers with postpartum depression (PPD). Individualized treatment plans target areas of the brain associated with mood regulation, ensuring optimal efficacy while minimizing side effects. This customization optimizes outcomes, providing targeted relief for PPD symptoms.
Bella Vida Proudly Supporting Women’s Mental Health
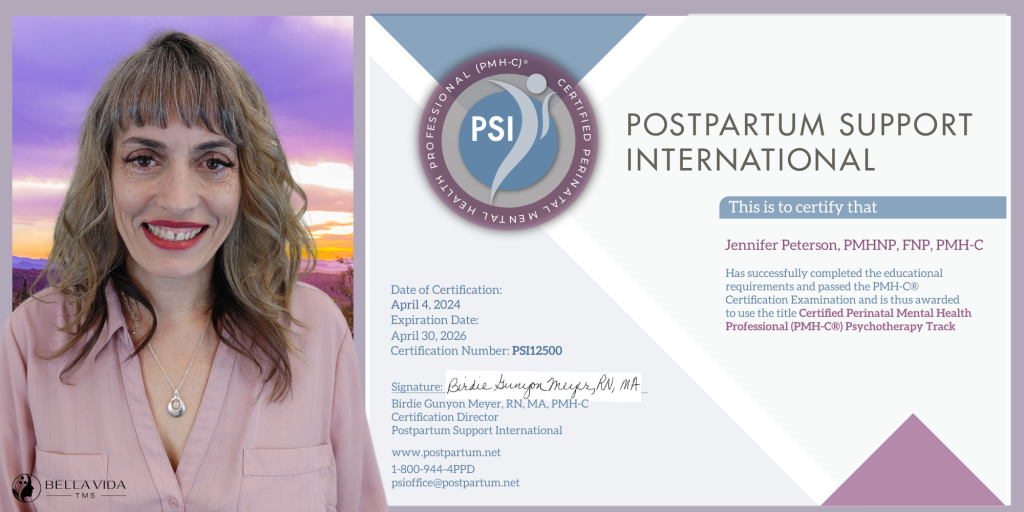
Bella Vida TMS is proud to announce that Jennifer Peterson, PMHNP, FNP, PMH-C, has recently received her Perinatal Mental Health Certification (PMH-C) in Psychotherapy. This significant achievement underscores her dedication to providing specialized care for pregnant and postpartum women experiencing mental health challenges. With this certification, Jennifer is now equipped with advanced knowledge and skills to support women during the perinatal period, which includes pregnancy and the first year postpartum.
At Bella Vida TMS, we understand the unique mental health needs of women during and after pregnancy. Postpartum depression is a common and often debilitating condition that can impact the well-being of both mother and child. With Jennifer’s new certification, we can now offer targeted and effective treatments, including Transcranial Magnetic Stimulation (TMS), to address postpartum depression. Jennifer Peterson’s expertise and our state-of-the-art TMS technology create a comprehensive approach to maternal mental health care at Bella Vida TMS.
External Reference links
- Neuropsychiatric Disease and Treatment – Effects of repetitive transcranial magnetic stimulation on clinical, social, and cognitive performance in postpartum depression
- Clinical TMS Society : – Maternal Mental Health and TMS-Part One: Transcranial Magnetic Stimulation in the Treatment Of Postpartum Depression (PPD)
- Transcranial magnetic stimulation for treatment of major depression during pregnancy: a review
- Translational Psychiatry – Mapping global prevalence of depression among postpartum women