Researchers have recently made a significant breakthrough in understanding cocaine use disorder (CUD) by identifying a robust functional connectivity brain signature. This discovery not only helps in accurately characterizing neural circuit abnormalities associated with CUD but also holds potential in predicting the response of CUD patients to repetitive transcranial magnetic stimulation (rTMS), a non-invasive brain stimulation therapy.
Cocaine Use Disorder: A Persistent Challenge
Cocaine use disorder is a condition marked by compulsive cocaine use and affects over one million Americans. According to SAMSHA, every year nearly 874,000 people are introduced to cocaine with the potential for a brain altering experience. Despite the availability of talk-based therapies, the high rate of relapse among CUD patients has driven researchers to explore more effective treatment options. In this context, brain imaging techniques have played a crucial role in uncovering the neurological underpinnings of CUD.
Previous studies using various brain imaging methods have revealed structural and functional differences in the brains of individuals with CUD compared to healthy controls. For instance, structural MRI scans have shown reduced grey-matter volume in several regions of the cerebral cortex. Additionally, scans measuring cumulative neural activity have identified patterns of heightened activation in the left dorsolateral prefrontal cortex (DLPFC) and bilateral occipital cortex among individuals craving cocaine.
The New Study: Unveiling Functional Connectivity
The new study, led by Drs. Yu Zhang and Kanhao Zhao of Lehigh University and reported in Nature Mental Health, took a novel approach by focusing on functional connectivity (FC) imaging. FC imaging examines how neurons connect and communicate across different brain regions under specific conditions, offering a more sensitive indicator of brain dysfunction compared to traditional imaging techniques.
Functional MRI (fMRI) scans have successfully established biomarkers for several neuropsychiatric disorders in the past. For example, elevated activity in presynaptic dopamine neurons in the brain’s striatum has been linked to antipsychotic treatment response in schizophrenia. Similarly, increased connectivity within the brain’s default mode network (DMN) has been associated with depression, and rTMS treatment has been observed to reduce DMN connectivity, leading to symptom improvement in depressed patients.
Building on these insights, the research team sought to identify a functional connectivity signature specific to CUD. To achieve this, they used machine learning algorithms to analyze resting-state fMRI scans from a “discovery” group comprising 71 CUD patients and 58 healthy controls. The signature they identified was then validated in an independent cohort of 81 CUD patients and 82 healthy controls.
A Landmark Discovery
The researchers succeeded in identifying a functional connectivity signature that was both accurate and specific in distinguishing individuals with CUD from healthy controls. This signature showed minimal false positives or negatives, underscoring its potential as a reliable biomarker for CUD. The successful replication of the results in an independent cohort further solidified the study’s findings.
The identified signature highlighted network-level abnormalities involving the frontoparietal control network (FPC), the default mode network (DMN), the dorsal attention network (DAN), and the ventral attention network (VAN). These findings are consistent with previous studies suggesting hyperconnectivity in brain regions associated with response inhibition in CUD patients. Additionally, the study provided evidence of reduced connectivity between the DMN and the limbic network (LIM), which was linked to cognitive complaints and anxiety in CUD patients.
The research team suggested that the hyperactivity observed in the limbic system of CUD patients might be counteracted by enhancing FPC activity, which tends to be pathologically suppressed in individuals with CUD. They also highlighted the medial prefrontal cortex (mPFC) as a promising treatment target for CUD, based on the observed connectivity patterns.
Implications for rTMS Treatment
One of the most significant findings of the study was the association between the identified functional connectivity signature and the response to rTMS treatment. The signature was specifically linked to the response to active rTMS, but not to the placebo treatment, indicating its potential utility in predicting which CUD patients may benefit from this therapy.
While rTMS has been experimentally administered for treating cocaine addiction, it is not yet approved by the FDA for this use. However, the study’s findings suggest that rTMS could be an effective treatment option for reducing craving in CUD patients, particularly by targeting the prefrontal cortex across the LIM, DMN, and FPC networks.
Future Directions
The researchers are optimistic about the future implications of their work. They propose that future studies should explore the possibility of directly manipulating dysfunctional brain circuits to address cocaine-craving symptoms. Additionally, further research is needed to determine whether the circuit dysfunctions captured by the newly identified functional connectivity signature have a causal connection with CUD.
This wasn’t the only study to find rTMS to be effective on CUD brain functions. In 2019, a research study also had outstanding results in rTMS Reduces Psychopathological Burden and Cocaine Consumption in Treatment-Seeking Subjects With Cocaine Use Disorder: An Open Label, Feasibility Study.
“ After four weeks of rTMS treatment, 9 out of 16 subjects (56.25%) had a negative urinalysis test, with a significant conversion rate with respect to baseline (Z = −3.00; p = 0.003). Craving scores significantly improved only at T2 (p = 0.020). The overall psychopathological burden, as measured by the SCL-90 Global Severity Index (GSI), significantly decreased during the study period (Z = −2.689; p = 0.007), with a relevant improvement with regards to depressive symptoms, anhedonia, and anxiety.”
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2019.00621/full
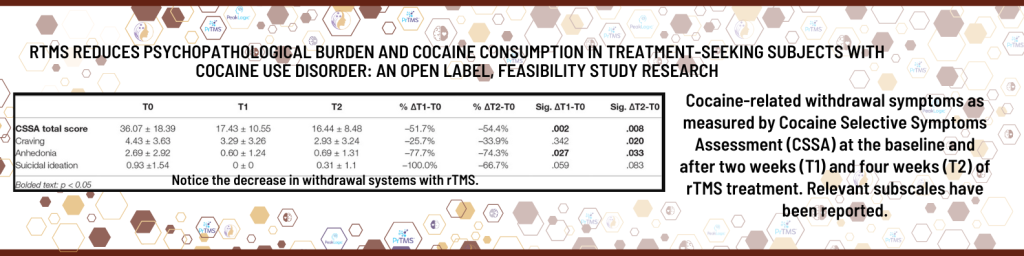
In Dr. Yu Zhang and Kanhao Zhao’s study and Dr. Pettorruso’s study, there was significant milestones in the quest to understand treat cocaine use disorder. The identification of a functional connectivity signature not only enhances our understanding of the neural circuits involved in CUD but also opens up new avenues for personalized treatment approaches, particularly through the use of rTMS therapy.
How TMS Works for CUD
Transcranial Magnetic Stimulation is a non-invasive treatment that uses magnetic fields to stimulate nerve cells in the brain. TMS is primarily used to treat depression, but recent studies suggest that it can also be effective for substance use disorders, including CUD.
Benefits of TMS for CUD
- Non-Invasive: Unlike some addiction treatments that require medication or invasive procedures, TMS is non-invasive and involves no surgery or anesthesia.
- Few Side Effects: TMS has minimal side effects, usually limited to mild discomfort at the treatment site or headaches, which often subside after a few sessions.
- No Systemic Effects: Because TMS works by directly stimulating brain regions rather than introducing chemicals into the body, it avoids systemic side effects that are common with medications.
- Short Sessions: TMS treatments are relatively quick, with sessions typically lasting 20-30 minutes, making it convenient for individuals with busy schedules.
The Future of CUD Treatment with TMS
While more research is needed to fully understand the long-term effects of TMS on Cocaine Use Disorder, the early results are encouraging. At Bella Vida TMS, we are committed to staying at the forefront of this innovative treatment approach and offering our patients the most advanced care available.
If you or someone you love is struggling with Cocaine Use Disorder, TMS might be the breakthrough treatment you’ve been searching for. Contact us today to learn more about how TMS can help you on the path to recovery.
External Reference links
- Brain and Behavior Research Foundation – Functional Connectivity Signature for Cocaine Use Disorder and Response to rTMS Brain Stimulation Therapy Is Identified
- NIH : – Developing Repetitive Transcranial Magnetic Stimulation (rTMS) as a Treatment Tool for Cocaine Use Disorder: a Series of Six Translational Studies
- Frontiers in Psychiatry- rTMS Reduces Psychopathological Burden and Cocaine Consumption in Treatment-Seeking Subjects With Cocaine Use Disorder: An Open Label, Feasibility Study