Crohn’s disease, a chronic inflammatory condition affecting the gastrointestinal tract, not only poses physical challenges but also exerts a significant toll on mental health. Individuals battling this condition often experience a range of psychological symptoms, including anxiety, depression, and diminished quality of life.
Crohn’s disease is a type of inflammatory bowel disease (IBD) that can affect different parts of the digestive tract and is often confused with the noninflammatory condition called Irritable Bowel Disease (IBD) aka Irritable Bowel Disease (IBS). Functional Bowel Disease (FBD) is a term for two conditions (Crohn’s disease and ulcerative colitis) that are characterized by chronic inflammation of the gastrointestinal (GI) tract.
Amidst the struggle, emerging therapeutic approaches like repetitive Transcranial Magnetic Stimulation (rTMS) offer promising avenues for alleviating the mental burden associated with Crohn’s disease, IBD and FBD.
The Psychological Impact of Crohn’s Disease
Crohn’s disease is characterized by inflammation of the digestive tract, leading to symptoms such as abdominal pain, diarrhea, fatigue, and weight loss. While the physical manifestations of the disease are well-documented, its impact on mental health is increasingly recognized as a crucial aspect of patient care. Research indicates a bidirectional relationship between Crohn’s disease and psychological well-being, wherein the symptoms of the disease exacerbate psychological distress, and vice versa.
Several studies have revealed that individuals with Crohn’s disease, IBD, and FBD exhibit higher rates of depression and anxiety compared to the general population. The chronic nature of the illness, coupled with unpredictable symptom flares and the necessity for lifelong management, contributes to heightened stress levels and emotional upheaval among patients. Moreover, the physical symptoms of Crohn’s disease often lead to social isolation, impaired functioning, and reduced quality of life, further exacerbating psychological distress.
Deep Dive into the Research: Article One
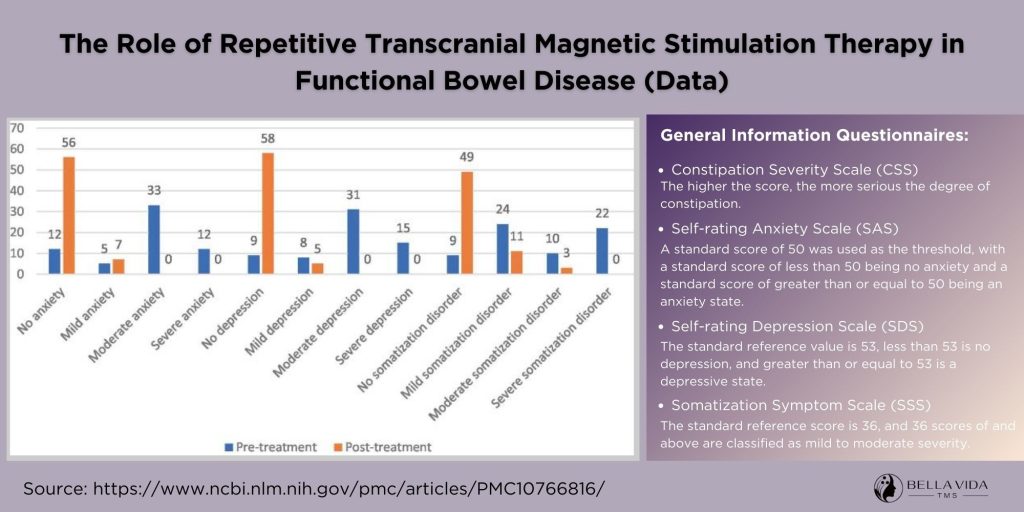
One research study of 226 subjects – Functional Bowel Disease (FBD) group (n = 113) and a healthy control group (n = 113) – received rTMS treatment sessions for their FBD. “The role of repetitive transcranial magnetic stimulation therapy in functional bowel disease” explores the potential therapeutic benefits of repetitive transcranial magnetic stimulation (rTMS) in managing functional bowel diseases. Functional bowel diseases, including conditions like irritable bowel syndrome (IBS), pose significant challenges to patients due to their complex symptomatology and often limited treatment options.
This scholarly investigation aims to explore the role of rTMS, a non-invasive neuromodulation technique, in alleviating the symptoms and improving the quality of life for individuals affected by functional bowel diseases. By examining the mechanisms of action, clinical efficacy, and potential neurobiological underpinnings of rTMS therapy, this study sheds light on novel approaches to addressing the multifaceted nature of gastrointestinal disorders from a neurocognitive perspective.
Chronic gastrointestinal discomfort poses significant challenges for patients, and over time, many develop psychological disorders and mental symptoms. Persistent anxiety and depression can impact the hypothalamus, vegetative nerves, and inhibit peripheral autonomic nerves, exacerbating intestinal discomfort and increasing the treatment burden.
Among them, anxiety disorders are the most common, with a prevalence of about 30–50%, followed by depression, with a prevalence of about 25–30%. In this study, among 113 patients with functional enteropathy, 17 (15.04%) had mild anxiety, 47 (41.59%) had moderate anxiety, and 38 (33.63%) had severe anxiety. There were 20 (17.70%) with mild depression, 48 (42.48%) with moderate depression, and 33 (29.20%) with severe depression.
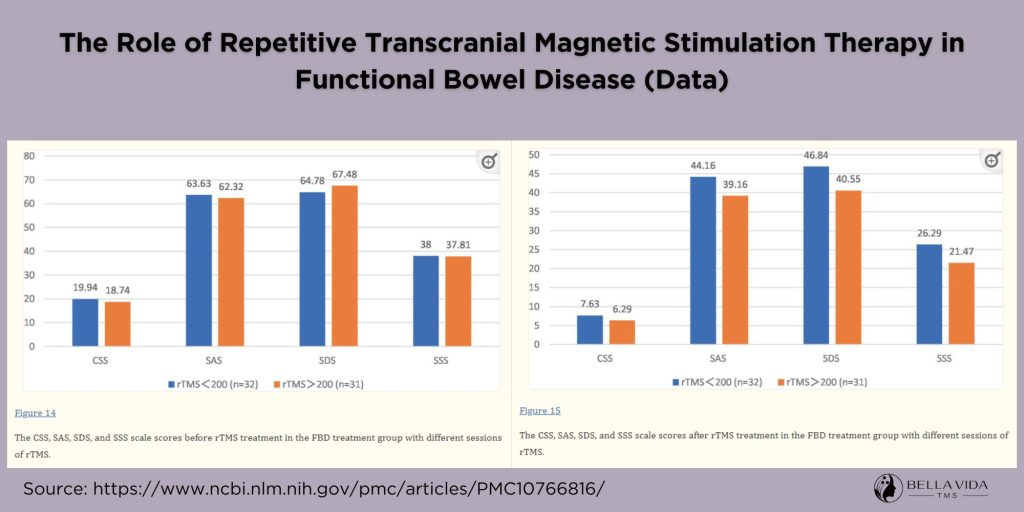
The effectiveness of rTMS treatment for patients with functional bowel disease was positively correlated with the number of treatments received. The images above of the data attests to the overall effectiveness. The use of rTMS for functional bowel disease has good patient compliance and acceptance, and provides rapid symptom relief with no significant adverse effects.
Deep Dive into the Research: Article Two
This research study “Clinical Application of Transcranial Magnetic Stimulation for Functional Bowel Disease” explores the therapeutic potential of transcranial magnetic stimulation (TMS) in managing functional bowel diseases, including conditions like irritable bowel Disease (IBD). This comprehensive investigation explores the application of TMS, a non-invasive neuromodulation technique, in modulating brain-gut interactions and alleviating gastrointestinal symptoms.
Through a thorough review of existing literature and clinical evidence, the study sheds light on the mechanisms of action underlying TMS interventions, the efficacy of different stimulation protocols, and the implications for patient care. By elucidating the role of TMS in targeting central nervous system pathways implicated in functional bowel diseases, this study contributes valuable insights to the burgeoning field of neurogastroenterology and holds promise for advancing the management of these challenging conditions.
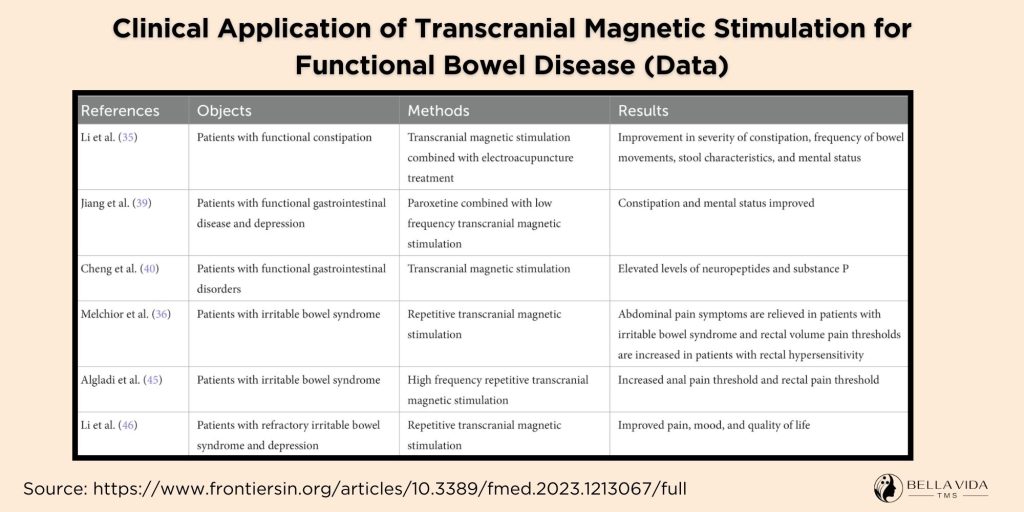
Given that Rome Committee classifies FBD into 6 different subtypes – Constipation, diarrhea, abdominal pain & discomfort, and anxiety, depression, and mental distress – this research breaks-down rTMS benefits found in the given studies. The table from the research simplifies whether TMS improved them. Below are excerpts from the research on how rTMS improved these areas:
Constipation:
Patients with functional constipation using TMS of motor evoked potentials (MEP) showed a significant decrease in MEP wave amplitude (reduced number of firing neurons) and a general increase in latency (slowed nerve conduction velocity). TMS therapy not only improves the patient’s constipation symptoms but also significantly reduces the patient’s mental state.
Abdominal pain & abdominal discomfort:
Research confirms that IBS is associated with changes in structural brain activity involved in pain processing. The application of repetitive low-frequency TMS increases the rectal pain threshold in patients with IBS, thereby reducing their abdominal pain symptoms. The analgesic effect of rTMS may be caused mainly by alterations in the central pain modulation system.
Anxiety & Depression:
More than half of the patients with constipation are accompanied by severe anxiety or depression. In the long term, in a state of high tension, anxiety can cause brain and intestinal axis dysfunction, which in turn aggravates the constipation condition, forming a vicious circle. TMS not only regulates the brain-gut axis disorder in patients with functional constipation but also significantly improves the patient’s anxiety and depression, which is more conducive to the treatment of constipation.
Pharmaceuticals: Increasing the Problem by Increasing the Severity of the Symptoms
Medications commonly prescribed for inflammatory bowel disease (IBD) and Crohn’s disease, such as certain types of opioids, can paradoxically exacerbate gastrointestinal symptoms, including constipation.
Opioids, often used to manage pain associated with these conditions, exert their effects by binding to opioid receptors in the gastrointestinal tract and the central nervous system. While they are effective in alleviating pain, opioids also slow down gut motility, resulting in delayed transit time and increased water absorption from the intestines, ultimately leading to constipation. Additionally, certain medications used to treat IBD, such as anticholinergics and tricyclic antidepressants, can have anticholinergic effects that further contribute to constipation by inhibiting smooth muscle contraction in the intestines.
Consequently, the use of these medications in the management of IBD and Crohn’s disease requires careful consideration of their potential impact on gastrointestinal function and the need for adjunctive therapies to mitigate constipation and ensure optimal symptom management.
Medication & Gut Flora
Medications prescribed for inflammatory bowel disease (IBD) and Crohn’s disease, while aimed at managing symptoms and reducing inflammation, can inadvertently disrupt the delicate balance of gut flora and impair functional digestion. One of the primary classes of medications used in the treatment of IBD and Crohn’s disease is immunosuppressants, such as corticosteroids, immunomodulators, and biologic agents.
These medications work by suppressing the immune response and reducing inflammation in the gastrointestinal tract. However, in doing so, they can also affect the composition and diversity of the gut microbiota, leading to dysbiosis—a condition characterized by an imbalance in the microbial community. Dysbiosis has been linked to various digestive disturbances, including impaired nutrient absorption, altered metabolism of dietary components, and increased intestinal permeability.
Antibiotics, often prescribed to manage bacterial overgrowth or infection in individuals with IBD, can further disrupt gut flora by indiscriminately targeting both harmful and beneficial bacteria. As a consequence of these medication-induced alterations in gut microbiota composition, functional digestion may be compromised, contributing to symptoms such as bloating, gas, abdominal discomfort, and irregular bowel movements.
While pharmacotherapy plays a crucial role in the management of IBD and Crohn’s disease, it is essential to consider the potential impact of these medications on gut flora and digestive function, and to explore complementary strategies for mitigating adverse effects on gastrointestinal health.
The Future for rTMS as a treatment for Crohn’s disease, IBD, and FBD
While the potential of rTMS in alleviating the psychological burden of Crohn’s disease is promising, further research is warranted to elucidate its long-term efficacy, optimal treatment protocols, and mechanisms of action. Large-scale randomized controlled trials are needed to establish the safety and efficacy of rTMS as a standard therapeutic intervention for addressing psychiatric comorbidities in individuals with Crohn’s disease, IBD, and FBD.
In clinical practice, the integration of rTMS into multidisciplinary treatment approaches for Crohn’s disease holds considerable promise for enhancing patient outcomes and improving overall quality of life. Collaborative efforts between gastroenterologists, psychiatrists, and neuroscientists are essential for advancing our understanding of the intricate interplay between gut health and mental well-being and developing personalized interventions tailored to the needs of individuals with Crohn’s disease.
Crohn’s disease exerts a profound impact on mental health, contributing to heightened rates of depression, anxiety, and diminished quality of life among patients. With more research, getting a clearer picture of how rTMS also affects the brain’s pathways that are altered due to IBM, FBD, and Crohn’s Disease may depict even more benefits to the treatment sessions.
Emerging therapeutic modalities such as rTMS offer a novel and promising approach for addressing the psychological sequelae of Crohn’s disease, providing hope for improved symptom management and enhanced well-being in affected individuals. Through continued research and innovation, we can strive towards comprehensive care that addresses both the physical and psychological dimensions of this complex chronic condition.
External Reference links
- National Institutes of Health – The role of repetitive transcranial magnetic stimulation therapy in functional bowel disease
- Frontiers in Medicine – Clinical application of transcranial magnetic stimulation for functional bowel disease
- Canadian Journal of Gastroenterology and Hepatology – Prevalence of Anxiety and Depression in Patients with Inflammatory Bowel Disease